- Home
- About Us
- Industry
- Services
- Reading
- Contact Us
U.S. Population Health Management Solutions Market: Current Analysis and Forecast (2025-2033)
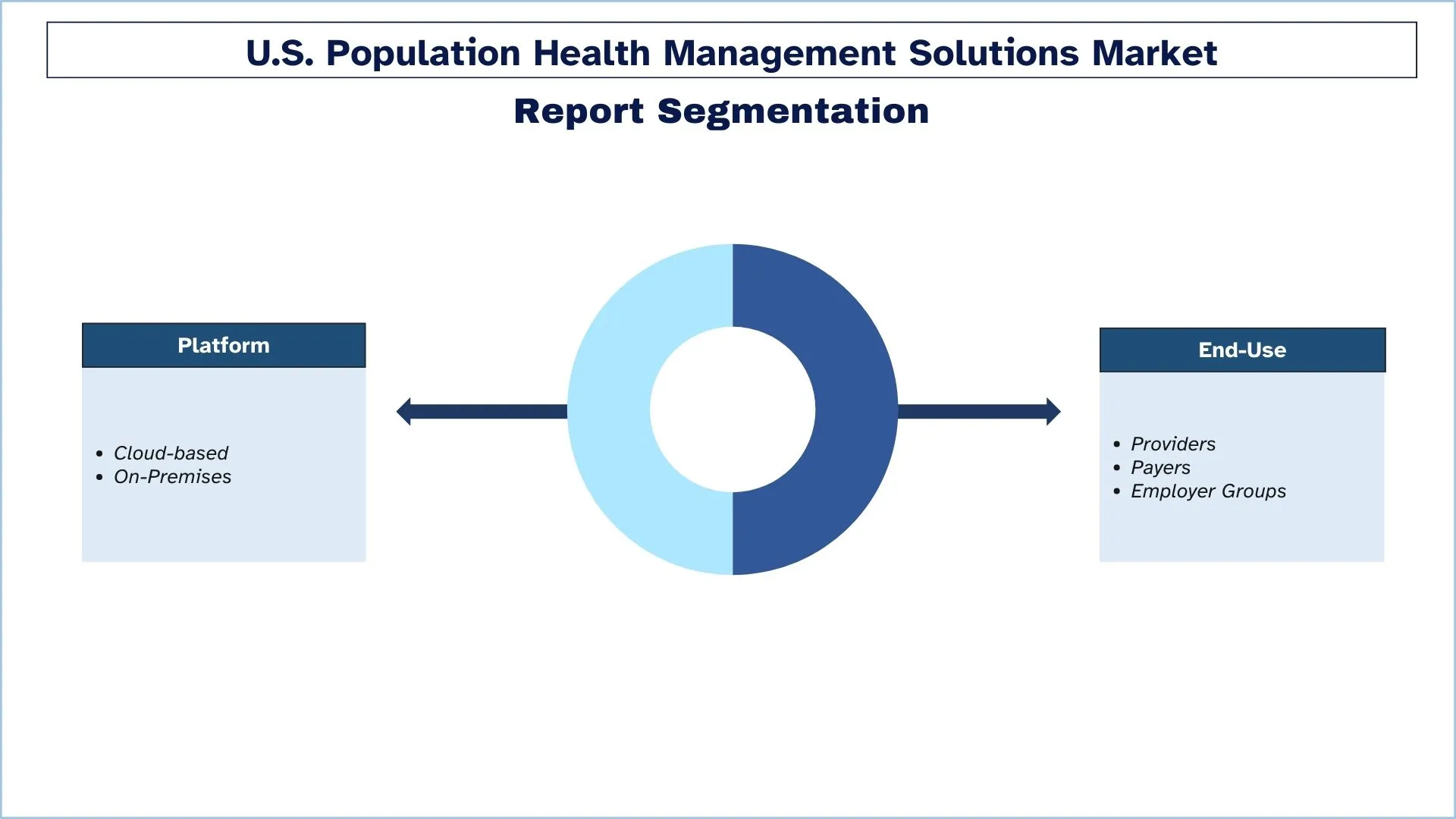
Emphasis on Platform (Cloud-based and On-Premises); End-Use (Providers, Payers, Employer Groups); and States
U.S. Population Health Management Solutions Market Size & Forecast
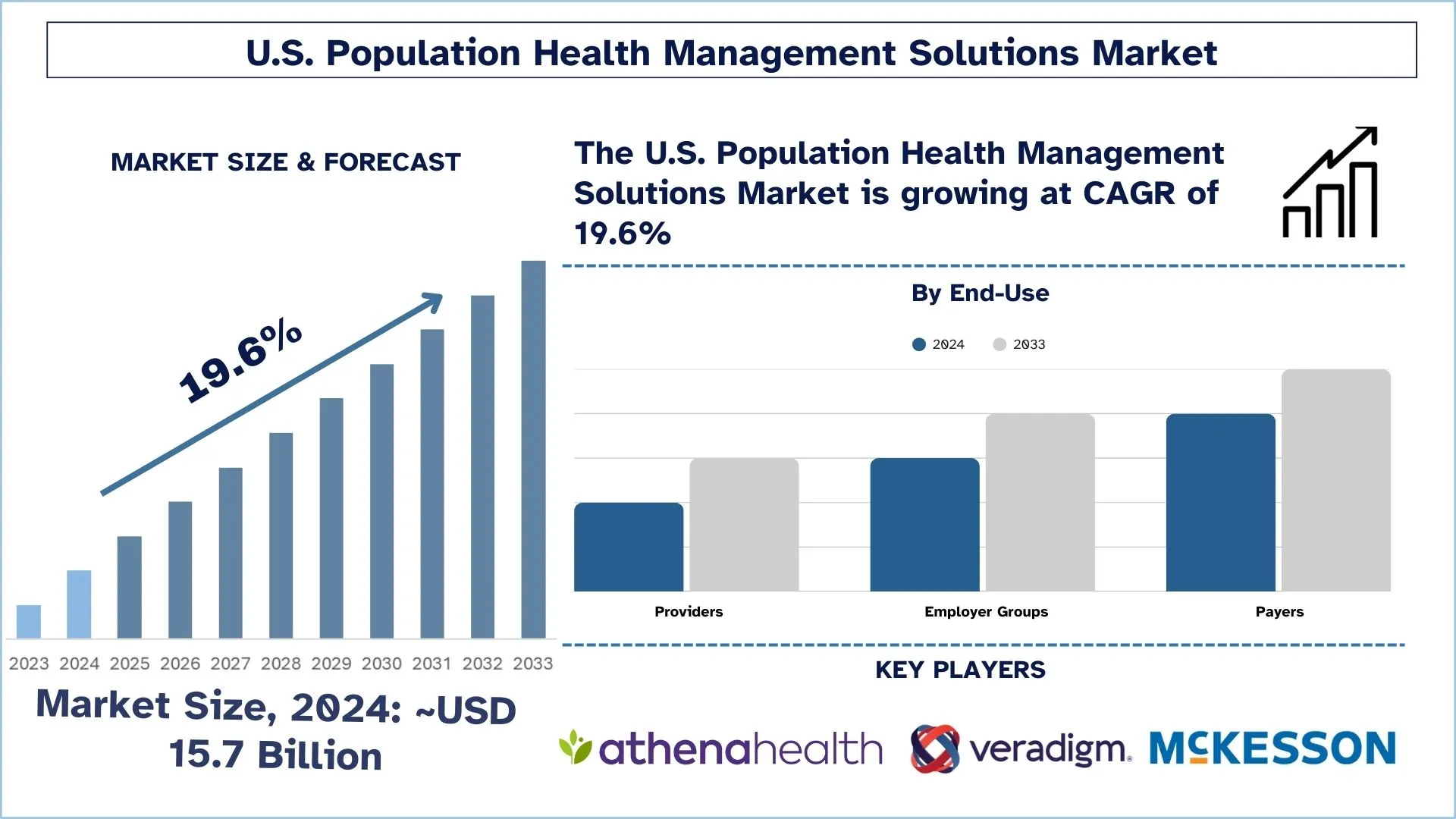
The U.S. Population Health Management Solutions Market was valued at approximately USD 15.7 billion in 2024 and is expected to grow at a substantial CAGR of around 19.6% during the forecast period (2025-2033), owing to the rising chronic disease burden and aging population.
U.S. Population Health Management Solutions Market Analysis
The population health management solutions market in the U.S. is a rapidly growing industry that is focused on improving the health and well-being of patient populations with technology and data analytics. Population health management solutions are designed to help healthcare providers manage patient populations, identify high-risk patients, and provide appropriate care to improve patient outcomes. The population health management solutions market in the U.S. is driven by several factors, including the increasing prevalence of chronic diseases, the need to manage healthcare costs, and the growing demand for remote patient monitoring and telemedicine services. Population health management solutions can help healthcare providers manage patient populations, identify high-risk patients, and provide appropriate care to improve patient outcomes.
U.S. Population Health Management Solutions Market Trends
This section discusses the key market trends influencing the various segments of the U.S. Population Health Management Solutions market as identified by our research experts.
Shift Toward Value-Based Care Models
Population Health Management Solutions in the U.S. market is undergoing a radical transformation because healthcare organizations are shifting toward value-based care models instead of traditional volume-based models. Healthcare providers and payers show increased interest in PHM platforms because this trend focuses on delivering preventive care and better patient results, together with improved cost-effectiveness. The solutions help perform real-time analysis and separate patients into groups, and manage coordinated care treatment while matching the requirements of value-based reimbursement. Organizations currently focus their investments on population-level tools combined with risk management systems and personalized care solutions to fulfill rising demands within value-focused healthcare systems.
U.S. Population Health Management Solutions Industry Segmentation
This section provides an analysis of the key trends in each segment of the U.S. Population Health Management Solutions market report, along with forecasts at the regional levels for 2025-2033.
The Cloud-Based Segment Holds the Largest Share of the U.S. Population Health Management Solutions Market.
Based on the platform, the market is bifurcated into cloud-based and on-premises. Amongst these, the cloud-based segment is expected to have a major share of the population health management solutions market in the U.S. during the forecast period. Cloud-based solutions offer several advantages over on-premises solutions, including lower upfront costs, scalability, and easier maintenance. Cloud-based solutions can be easily scaled up or down based on the needs of the user, and the provider is responsible for maintaining the infrastructure, which can save healthcare providers time and resources. Cloud-based solutions offer greater flexibility and accessibility, as they can be accessed from anywhere with an internet connection. This can be particularly important for rural and remote areas where access to healthcare providers may be limited.
The Payers Segment is Expected to Witness a Higher CAGR than the U.S. Population Health Management Solutions Market.
Based on end-use, the market is segmented into providers, payers, and employer groups. Among these, payers are expected to have a major share of the population health management solutions market in the U.S. during the forecast period. The payers segment will have a major share of the market during the forecast period. Payers, such as health insurance companies and government agencies, play a critical role in population health management as they are responsible for funding healthcare services. Payers are interested in population health management solutions that can help to reduce healthcare costs, improve patient outcomes, and increase access to care.
California has a significant share of the market in 2024.
The Population Health Management (PHM) Solutions market in California experiences significant changes because of state-level efforts to improve health services and patient outcomes. The Department of Health Care Services (DHCS) has initiated the Population Health Management Program through its CalAIM initiative. The Population Health Management program of Medi-Cal members delivers a complete personalized health approach that focuses on better results and equal treatment opportunities for all populations, including children and pregnant people, and both elderly groups and disabled persons. The initiative demonstrates California's dedication to uniting care management systems with patient engagement tools and electronic health records for the establishment of a unified healthcare structure. The emphasis on preventive medicine, together with disparity solutions, will position California as an example in population health management to create an efficient and equitable healthcare system.
U.S. Population Health Management Solutions Industry Competitive Landscape
The U.S. Population Health Management Solutions market is competitive, with several global and international players. The key players are adopting different growth strategies to enhance their market presence, such as partnerships, agreements, collaborations, new product launches, geographical expansions, and mergers and acquisitions.
Top U.S. Population Health Management Solutions Companies
Some of the major players operating in the market are Veradigm Inc.; Cerner Corp. (Oracle); Conifer Health Solutions, LLC (Tenet Healthcare); EClinicalWorks; Enli Health Intelligence (Cedar Gate); McKesson Corp.; Medecision (Health Care Service Corporation (HCSC)); Optum, Inc. (UnitedHealth Group); Koninklijke Philips N.V.; athenahealth, Inc. (Bain Capital and Hellman & Friedman)
Recent Developments in the U.S. Population Health Management Solutions Market
In April 2022, Medecision, a leading name in digital care management, announced the initiation of a strategic partnership with Clearstep Health to pioneer enhanced patient engagement for existing as well as new health plans and systems.
U.S. Population Health Management Solutions Market Report Coverage
Report Attribute | Details |
Base year | 2024 |
Forecast period | 2025-2033 |
Growth momentum | Accelerate at a CAGR of 19.6% |
Market size 2024 | USD 15.7 Billion |
Major contributing region | California is expected to grow at the highest CAGR during the forecasted period. |
Key regions covered | California, New York, Florida, Washington, Texas, Rest of U.S. |
Companies profiled | Veradigm Inc.; Cerner Corp. (Oracle); Conifer Health Solutions, LLC (Tenet Healthcare); EClinicalWorks; Enli Health Intelligence (Cedar Gate); McKesson Corp.; Medecision (Health Care Service Corporation (HCSC)); Optum, Inc. (UnitedHealth Group); Koninklijke Philips N.V.; athenahealth, Inc. (Bain Capital and Hellman & Friedman) |
Report Scope | Market Trends, Drivers, and Restraints; Revenue Estimation and Forecast; Segmentation Analysis; Demand and Supply Side Analysis; Competitive Landscape; Company Profiling |
Segments Covered | By Platform, By End-Use, By Region/Country |
Reasons to Buy the U.S. Population Health Management Solutions Market Report:
The study includes market sizing and forecasting analysis validated by authenticated key industry experts.
The report presents a quick review of overall industry performance at a glance.
The report covers an in-depth analysis of prominent industry peers with a primary focus on key business financials, product portfolios, expansion strategies, and recent developments.
Detailed examination of drivers, restraints, key trends, and opportunities prevailing in the industry.
The study comprehensively covers the market across different segments.
Deep dive regional-level analysis of the industry.
Customization Options:
The U.S. Population Health Management Solutions market can be customized further as per the requirement or any other market segment. Besides this, UnivDatos understands that you may have your own business needs; hence, feel free to contact us to get a report that completely suits your requirements.
Table of Content
Research Methodology for the U.S. Population Health Management Solutions Market Analysis (2023-2033)
We analyzed the historical market, estimated the current market, and forecasted the future market of the U.S. Population Health Management Solutions market to assess its application in major regions worldwide. We conducted exhaustive secondary research to gather historical market data and estimate the current market size. To validate these insights, we carefully reviewed numerous findings and assumptions. Additionally, we conducted in-depth primary interviews with industry experts across the U.S. Population Health Management Solutions value chain. After validating market figures through these interviews, we used top-down and bottom-up approaches to forecast the overall market size. We then employed market breakdown and data triangulation methods to estimate and analyze the market size of industry segments and sub-segments.
Market Engineering
We employed data triangulation techniques to finalize the overall market estimation and derive precise statistical numbers for each segment and sub-segment of the U.S. Population Health Management Solutions market. We split the data into several segments and sub-segments by analyzing various parameters and trends, including platform, end-use, and regions within the U.S. Population Health Management Solutions market.
The main objective of the U.S. Population Health Management Solutions Market Study is to
The study identifies current and future trends in the U.S. Population Health Management Solutions market, providing strategic insights for investors. It highlights regional market attractiveness, enabling industry participants to tap into untapped markets and gain a first-mover advantage. Other quantitative goals of the studies include:
Market Size Analysis: Assess the current and forecast market size of the U.S. Population Health Management Solutions market and its segments in terms of value (USD).
S. Population Health Management Solutions Market Segmentation: The study segments the market by platform, end-use, and region.
Regulatory Framework & Value Chain Analysis: Examine the regulatory framework, value chain, customer behavior, and competitive landscape of the U.S. Population Health Management Solutions industry.
Regional Analysis: Conduct detailed regional analysis for key areas such as California, New York, Florida, Washington, Texas, Rest of the U.S.
Company Profiles & Growth Strategies: Company profiles of the U.S. Population Health Management Solutions market and the growth strategies adopted by the market leaders to sustain the fast-growing market.
Frequently Asked Questions FAQs
Q1: What is the U.S. Population Health Management Solutions market's current size and growth potential?
As of 2024, the U.S. Population Health Management Solutions market is valued at approximately USD 15.7 billion and is expected to grow at a CAGR of 19.6% through 2033.
Q2: What are the driving factors for the growth of the U.S. Population Health Management Solutions market?
The growing prevalence of chronic conditions like diabetes, heart disease, and an aging demographic is fueling demand for PHM solutions that enable proactive, coordinated care.
Q3: Which segment has the largest share of the U.S. Population Health Management Solutions market by end-use?
The payers segment currently holds the largest market share in the end-use segment.
Q4: What are the major trends in the U.S. Population Health Management Solutions market?
Healthcare providers are increasingly adopting population health management tools to support value-based care, focusing on preventive care, patient engagement, and outcome-driven reimbursement.
Q5: Which region will dominate the bone sonometer market?
California leads the U.S. Population Health Management Solutions market.
Q6: What are the biggest challenges in the U.S. Population Health Management Solutions market?
Fragmented healthcare systems and a lack of standardized data formats make it difficult to integrate patient information across providers, limiting the effectiveness of population health strategies.
Q7: Who are the Top players in the U.S. Population Health Management Solutions market?
The leading companies driving innovation in U.S. Population Health Management Solutions include:
• Veradigm Inc.
• Cerner Corp. (Oracle)
• Conifer Health Solutions, LLC (Tenet Healthcare)
• EClinicalWorks
• Enli Health Intelligence (Cedar Gate)
• McKesson Corp.
• Medecision (Health Care Service Corporation (HCSC))
• Optum, Inc. (UnitedHealth Group)
• Koninklijke Philips N.V.
• athenahealth, Inc. (Bain Capital and Hellman & Friedman)
Q8: What are the key technological innovations shaping the U.S. Population Health Management Solutions market?
Emerging technologies such as AI-driven analytics, cloud-based platforms, and real-time data integration are revolutionizing PHM solutions. These innovations enable better risk stratification, predictive modeling, and more personalized, data-informed care plans that align with value-based care models.
Q9: How can investors evaluate high-potential opportunities in the U.S. PHM Solutions market?
Investors should assess companies with scalable platforms, strong partnerships with payers and providers, regulatory compliance readiness, and proven outcomes in care coordination and cost reduction. Focused investments in AI, interoperability, and patient engagement tools offer significant growth potential.
Related Reports
Customers who bought this item also bought